Lungs & Chest
Healing Mists
The Aerosol Lab
Aerosol science has been a mainstay of respiratory research at St. Joseph’s Healthcare Hamilton for decades thanks to the work of some incredibly talented clinicians, scientists, and engineers. As the Firestone Institute for Respiratory Health approaches its 45th anniversary, we’re reflecting on some major achievements from the Firestone’s Aerosol Research Laboratory.
An Early Milestone
In the late 1970s, a team of aerosol researchers were working on methods to improve the efficacy and safety of metered dose inhalers (MDIs), used to treat a variety of airway diseases such as asthma, COPD, and others. Their solution to the challenges presented by early inhalers was to design and validate a new medical device called a valved holding chamber, or spacer.
Spacers work by separating the inhaler process into two discrete steps. First, the user releases the medication into the spacer chamber via the one-way valve where the useful portion is retained. Then the user can inhale the medication when they are ready and at their preferred pace. By slowing down the speed of the aerosol coming from the inhaler, the device effectively increases the amount of medication in smaller particles through the physical mechanisms of evaporation and impaction. It is this finer aerosol that makes it into the lungs instead of hitting the back of the throat. For patients taking inhaled corticosteroids, long-term use of the spacer led to a decrease in oral fungal infections (thrush).
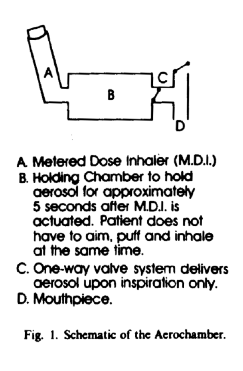
A schematic drawing of the AeroChamber device.
These devices are particularly helpful for those who are unable to take deep breaths, as well as those who are unable to synchronize their breathing with the release of medication from the inhaler. The design was first described in 1980 in the journal American Review of Respiratory Diseases.
Now sold by Trudell Medical Group, their invention has since become known globally as the AeroChamber®. This device continues to benefit patients, helping them successfully take aerosol medications for the treatment of asthma, COPD, and other respiratory diseases.
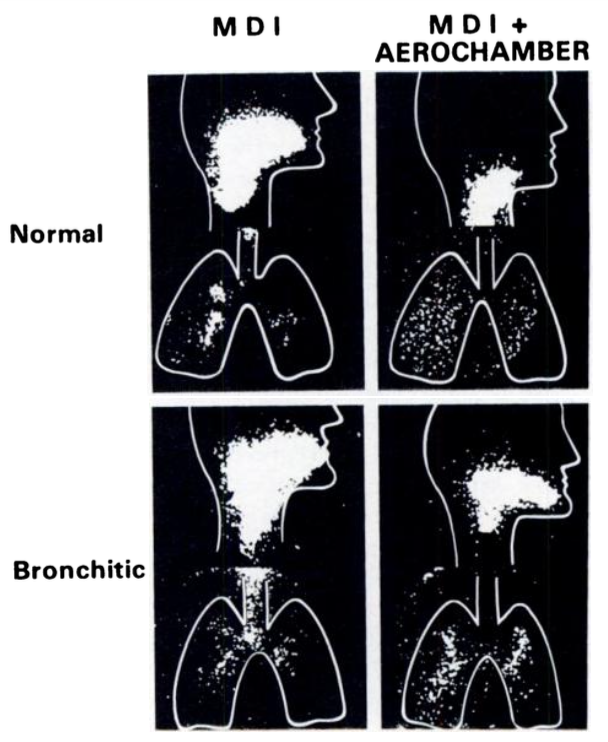
(Left) A gamma camera (scintiscan) was used to show the relative particle distribution after inhaling from a metered-dose inhaler alone (left column) compared to an MDI with the AeroChamber (right column). The top and bottom rows are comparing healthy lungs versus the lungs of patients with COPD. Outlines of the head and lungs are superimposed over the photos.
(Source: Dolovich, M., Ruffin, R., Corr, D., & Newhouse, M. T. (1983). Clinical evaluation of a simple demand inhalation MDI aerosol delivery device. Chest, 84(1), 36–41. https://doi.org/10.1378/chest.84.1.36)

The Aerosol School
In 2009, Myrna Dolovich was having difficulty finding technicians qualified to work in the Aerosol Lab. An engineer by training, Dolovich conducts research focused on inhalation therapy and drug delivery devices for medical aerosols – medicines that prevent, treat, or assess lung diseases such as tuberculosis, asthma, COPD, and others.

Dolovich leads a workshop during the Aerosol School in St. Joe’s Campbell Auditorium.
Recognizing the need for basic training in pharmaceutical aerosols, she set to work organizing a course to teach this needed skillset. With faculty composed of Canadian and American aerosol experts from academia and the pharmaceutical industry, the Aerosol School was born.
The Aerosol School is a three-day teaching program, led by Myrna Dolovich, that offers expert training and information in the field of medical aerosols.
The course teaches a range of measurements, techniques, and approaches to drug development and inhaler design used in academic and pharmaceutical industry laboratories. The participants also explore clinical applications ranging from the ambulatory settings to critical care.
From there, says Dolovich, “they should be able to take the next steps on their own.”
Now in its eleventh year, the Aerosol school has over 250 students from around the world who have completed the training. By fostering a unique learning environment, Dolovich is helping to ensure that aerosol research in medicine thrives.
Inhaled Vaccines
When the COVID-19 pandemic hit, researchers around the world began working on new vaccines to boost immunity and ultimately save lives. Vaccines can made using new technologies, like mRNA, were seen alongside more common methods, such as viral vector, live attenuated, and inactivated vaccines. There are other variations as well, such as the delivery method – intra-muscular injection has been common for COVID-19 and many other vaccines, but what if you could deliver a vaccine to where it was needed most?
The respiratory mucosal immune system is the body’s first line of defence for airborne pathogens. Because of this, researchers have been working on methods to deliver vaccines directly into the lungs.
Prior to the pandemic, researchers at McMaster University, including scientists at the Firestone’s Aerosol Lab, were working on an inhaled vaccine for tuberculosis. They conducted a Phase 1B clinical trial examining the efficacy and safety of a low-dose and high-dose inhaled vaccine, compared to the same vaccine given by intra-muscular injection.
Dolovich worked to characterize the aerosol device and droplets for the study, which found that a low-dose aerosol vaccine is a superior way to elicit immunity against tuberculosis. Researchers have since demonstrated that other respiratory pathogens, such as COVID-19, have similar benefits when using an inhaled vaccine as compared to an intra-muscular injection.
As of November 2022, researchers at McMaster are developing a second-generation COVID-19 inhaled vaccine, with help from clinicians, scientists, and engineers at the Firestone Institute.
Whether it’s developing medical devices that improve safety and efficacy of inhaled medications, training the next generation of scientists on the intricacies of aerosol research, or working with partners at McMaster and beyond to develop ground-breaking vaccines for respiratory diseases, the Aerosol Research Laboratory continues to contribute to medical advancements in respirology.